Hand surgery
- Carpal tunnel syndrome
- Trigger finger
- Inflammation of the thumb tendon sheath
- Synovial cyst (Ganglion)
- Dupuytren’s contracture
Nerve constriction (Carpal tunnel syndrome)
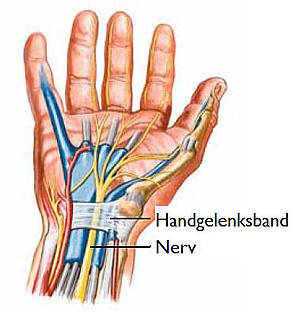
The cause of the so-called carpal tunnel syndrome is a constriction of a major nerve in the narrow passage of the wrist. The nerve, accompanied by the finger flexor tendons, passes through a narrow canal, bordered on 3 sides by wrist bones and on top by a tight transverse carpal ligament. Causes for a spatial imbalance in this carpal tunnel may be poorly healed fractures, a thickening of the wrist band, swelling or growths. However, in most cases, there is no pathological change, and the carpal tunnel syndrome is said to be of unknown cause. Women are frequently affected, and often on both sides.
Typical indications of carpal tunnel syndrome are nocturnal formications (“pins and needles”) in the affected hand. The patient is awakened by a tingling or prickling pain in the early morning hours—often in the thumbs, index finger, middle finger and half of the ring finger.
It is also described by complaints of clumsiness in buttoning and unbuttoning, sewing or picking up small objects. In later stages, complaints of decline in gross motor function are typical, and this is visible as a regression of the muscle tissue of the thumb joint.
The diagnosis is confirmed by a measurement of nerve conduction speed. The recommend conservative measure of immobilization with wrist support rarely has a long-lasting success even in less severe cases with minimal pain. Cortisone injections are strongly discouraged, as these can actually increase the pain over the long term.
If a carpal tunnel syndrome does not improve after 3 months of wearing a wrist support and the patient is still suffering from the pain, an operation is advisable. We perform the procedure on an outpatient basis and with regional anesthetic. The transverse carpal ligament is split lengthwise by making an approximately 3 cm long, L-shaped incision within the skin fold lines. This gives the flattened and compressed nerves in this area space to recover.
In the first few days after an operation, you should protect the affected hand and keep it elevated (arm sling). The fingers should be moved regularly without load, and after a few a days, light activity can resume. The stitches are removed after around 10-14 days, and more intensive activity is possible again after 2-4 weeks. For extreme stresses (e.g. heavy construction work), a recovery time of 4-6 weeks is to be expected. The longer the pain and constriction of the nerves lasted before, the longer the time for a complete recovery of the nerves.
Trigger finger
Trigger finger is a matter of a circumscribed thickening of a finger flexor tendon and a narrowing ring band in the palm region. The sliding of the tendon through the ring band (a kind of “strap”) is hampered or impeded. Causes of trigger finger include a longer-term overstressing in the palm area by thin, hard objects (e.g. pliers, hedge trimmers, etc.) or wear and tear. The mostly frequently affected fingers are the ring and middle fingers, but also often the thumbs. The disorder usually appears in the 50s and is three times more common in women.
Patients complain that the affected finger gets stuck when they bend it. In the early stages, the patient can overcome this blockage by using increased force, during which the characteristic snap occurs during the movement and stretching. Later, the affected finger remains fixed in the bending or stretching position.

The treatment is basically an operation, and cortisone injections should be avoided. The ring band is revealed by making an approximately 1.5 cm long skin incision under regional anesthetic and is split, while protecting the nerves. The adequacy of the split is assessed by the mobility of the tendon. A special follow-up is not required, but early, active movement of the affected finger is important.
Inflammation of the thumb tendon sheath
A painful irritation of the thumb tendon sheath tissue that extends over the wrist is the symptom of de Quervain tendon sheath inflammation. The pain emerges gradually, radiating in the direction of the thumb and along the forearm and increases upon gripping or holding objects. Because measures such as immobilization or even cortisone injections only seldom permanently eliminate the pain, an early decision for an operation saves the patient a lifetime of suffering.
To expose the thickened thumb tendon sheath compartment, a skin incision is made under regional anesthetic in the area of the thumb side of the wrist (on the side of the “Tabatière”). While protecting the nerves, this tendon compartment is now split, so that the tendon can glide freely again. The healing process usually takes a few days, and the thumb should be actively moved on a regular basis after the surgery.
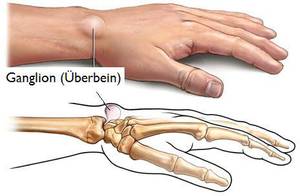
Synovial cyst (Ganglion)
Ganglia are round bulging elastic nodes in the vicinity of joints (frequently the wrist) and tendon sheaths. Because of their swelling consistency, ganglia are also commonly referred to as “cysts”. Sometimes ganglia are the result of accidents, but usually they are real, always benign neoformations in terms of an evagination of the articular capsule. The pain depends on the size of the ganglion and the proximity to tendons, nerves and joints. Thus, the complaints are of a weakness in the wrist area, dull pain or even paralysis.
Ganglia can occasionally disappear on their own. An operation is indicated if the ganglion bothers the patient for cosmetic reasons or if the patient is sensitive to the pain. Previously, ganglia were crushed or dug out, and occasionally cortisone injections were used. All these treatments share the disadvantage that sooner or later the ganglion will regenerate, because with these methods the covering membrane is not removed. Thus, the radical operative removal is the method of choice for treatment of ganglia.
The surgery takes place under regional anesthesia, and the ganglion is worked free and removed through a small skin incision made directly above the node, while protecting the blood vessels and nerves. Afterwards, the hand should be taken care of for several days, and light activities can be resumed after 2-3 days, while heavier stresses can be added after about 2-3 weeks. In about 10 – 15 % of cases, even with radical surgery, you may see the ganglion regenerate after a few months or even after a few years, so that another operation is required.
Dupuytren’s contracture

The case of a gnarled or callus-type thickening of the surface of the palm is designated as a so-called Dupuytren’s Contracture, named after the man who discovered it, the French Baron Guillaume Dupuytren (1777-1835). This pathological deformation of the connective tissue in the palm of the hand is often only noticed in an advanced stage. First signs of this disease are knotty nodes that can be felt under the skin of primarily in male patients. Generally, there is no pain. In its continued progression, it could be that several more or less thick strands are formed on the tissue bands leading to the finger joints. Sometimes these strands contract so strongly that the affected fingers can no longer be extended.
The cause of this disease is unknown, but a tendency in families as well as a connection to diabetes and liver diseases is prevalent. The surgery is the only sensible treatment. The operation should be performed either when pain exists, the patient feels hampered in his functionality or if one or more fingers can no longer be fully extended.

If the gnarled thickening is not too extensive, no more than 2 fingers are affected and the ability to extend the finger not overly limited, then the operation can be performed on an outpatient basis. However, a requirement is also the social environment at home and the necessity of a household help organized, mostly for older patients. It is important for patients to be informed of the risks of complications such as nerve damage or wound healing disorders. They must also be aware that sometimes the treatment period after the operation can last up to several weeks, that a full extension of the affected finger does not always result and that sometimes the condition can reoccur. Depending on the situation, a physiotherapy treatment is also required after the surgery.
The gnarled thickening and strands are loosened and cut out during the operation, while taking greatest care to protect the main nerves and blood vessels. Depending on the situation, longer skin incisions are required, sometimes in a Z-formation, so that the wound can be sealed again with the fingers straightened. Strict elevation is advisable in the first few days at home, and the operated finger should be passively fully extended several times per day.